Save articles for later
Add articles to your saved list and come back to them any time.
Australia is in the grip of an eighth COVID wave, but health officials remain confident in their decision to end the country’s emergency response, arguing the nation will now take a “new business as usual” approach.
Infectious disease experts and doctors say the pandemic has left the world with a new and nasty respiratory virus that will challenge health systems indefinitely. But they agree Australia is past the emergency phase, with the latest wave of infections predicted to be less severe than before.
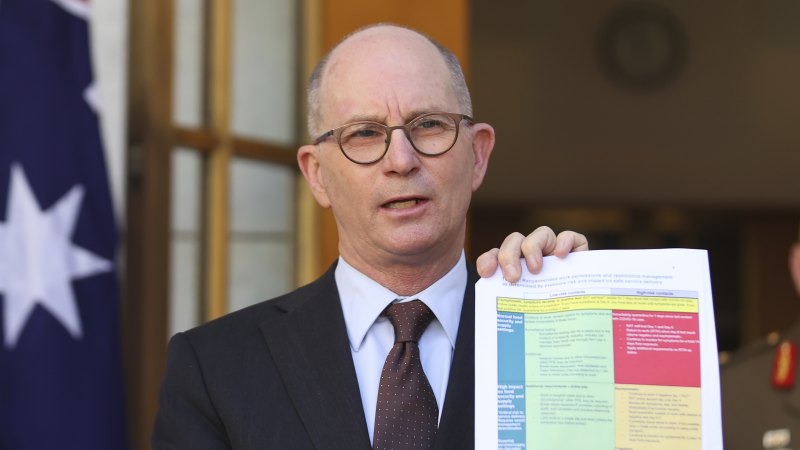
Chief Medical Officer Paul Kelly says Australia is now well protected by immunity built up through vaccinations and previous infections.Credit: Rhett Wyman
The country’s chief medical officer, Professor Paul Kelly, said when it recently became clear Australia was in another COVID-19 wave that he wondered whether it was the right time to end the classification of COVID as a Communicable Disease Incident of National Significance (CDINS).
However, he said he and state chief health officers agreed they would go ahead and issue an October 20 statement heralding an end to the nation’s COVID-19 emergency response.
Kelly said Australia was now well protected by immunity built up through millions of vaccinations and previous infections, and could afford to shift to a “new business as usual” response to COVID.
“Each of the waves we’ve had this year have been less and less severe,” said the chief medical officer in an interview this week.
“There’s still a possibility that we could have a brand new variant of concern, but when we look at what’s happened since late 2021 when Omicron came into being … we’ve had literally hundreds of subvariants … of Omicron, but nothing’s really pushed ahead in a different way.”
Kelly said the end of the CDINS declaration would have no significant impact on the management of the disease in Australia, but the National Incident Centre in Canberra, which had been running since 2019 through a number of disasters, has been closed for the first time in more than four years.
From this month, national COVID data will be reported monthly rather than weekly.
There were 1239 Australians hospitalised with COVID-19 last Friday – the highest number since July, though well down on the earlier winter COVID wave, which peaked at 2771 hospitalisations in early June. Just over 3375 deaths were caused by COVID in the first nine months of this year in Australia, compared with 8622 over the same period in 2022, Australia’s deadliest pandemic year.
Professor James McCaw, one of Australia’s top pandemic advisers, said observers had seen the latest COVID wave coming for about a month.
He said it was not yet possible to predict when it would peak, noting that because it was rising slowly, it would also decrease slowly.
“We don’t expect notifications or, more importantly, hospital numbers to get too much higher or too high,” he said.
The mathematical biologist and epidemiologist said it was a sensible time for an official end to the emergency response, but said it was important that Australia maintained its pandemic improvements in monitoring infection spread, and expand them to other pathogens such as the flu.
“The sad, unavoidable fact is the world is now a slightly more dangerous place because not only is influenza circulating, but so is SARS-COV-2,” he said.
GP registrar Dr Ashley Van Leeuwestyn, who works on the NSW Central Coast, said she started noticing an uptick in COVID diagnoses about three or four weeks ago.
It was being detected in patients of all ages, she said, but the hardest hit were older people with respiratory conditions such as chronic obstructive pulmonary disease. A small number have required hospitalisation for oxygen and other support.
Van Leeuwestyn said many patients think COVID is “gone”. In reality, it’s one of the key conditions she is considering when people see her with a range of different symptoms, from fevers to gastrointestinal upset.
“It’s a new normal,” she said. “A couple of years ago, we didn’t know anything about it … now it’s a big part of lots of presentations.”
McCaw stressed that the elderly and other vulnerable groups should be up to date with their booster vaccines.
It is a view shared by Kelly, who urged people not to wait for new vaccines to arrive.
“My clear message is, if you’re in those vulnerable groups, the best vaccine you can get is the one that’s available for you today,” he said.
The latest vaccine recommendation is for everyone aged 75 or older to receive a COVID booster if it has been more than six months since their last vaccination.
Those aged over 64 and younger adults who are severely immunocompromised should also have a discussion with their doctor about whether a booster might be suitable for them.
Kelly also said people in vulnerable groups should speak to their GPs about their plan to get oral antivirals immediately after they test positive to COVID (all those aged 70 or over are eligible for the medication, regardless of their risk factors).
This week, Melbourne GP Dr Vyom Sharma had his last shift at a general practice respiratory clinic that is no longer funded by government. He can’t remember the last time he sent a COVID-19 patient to hospital, but emphasised it remains a costly disease for many.
“We’ve just had some … quite robust research come out showing that the percentage of people who are getting long COVID is sitting at about 3 per cent,” he said.
Sharma was recently reinfected with COVID. He had to take four days off work. It meant patients at two aged care facilities could not be seen, and about 60 GP patients missed appointments.
The health commentator said he was seeing positive trends in people being allowed to work from home while sick, but stressed the importance of staying away from others when you have respiratory symptoms.
“I think that’s something we should absolutely retain and, frankly, [it] shouldn’t really take COVID to teach us that.”
Australian virologist Associate Professor Kirsty Short also caught COVID recently, for the first time.
“Any time I tried to do something, I would just get a fever … I’d hate to think what it would have been like if I hadn’t been vaccinated.”
Short said there was a hope early in the pandemic that COVID would quickly settle into a seasonal virus like influenza, where there was typically one large wave each year. Instead, the most recent pattern in Australia had been at least two waves every 12 months, peaking in winter and summer.
“I’m not sure we’ll fit that all into a seasonal pattern in the next year or so. I think that might take longer than that.”
The Morning Edition newsletter is our guide to the day’s most important and interesting stories, analysis and insights. Sign up here.
Most Viewed in National
From our partners
Source: Read Full Article